Expert shoulder care at your fingertips
You’re tired of living with chronic shoulder pain, but you want to avoid any unnecessary procedures. With access to the country’s best shoulder experts, you can get back to doing the activities you love.
Feel completely confident in your journey toward shoulder health
Whether you need a second opinion or you’re just starting out, it’s time to work with a shoulder specialist at Best In Class MD. Find your condition or recommended treatment below and see how we can help.
This list contains some of our most commonly seen conditions, but it is by no means exhaustive. Our shoulder doctors handle the same wide variety of conditions that an in-person physician would.
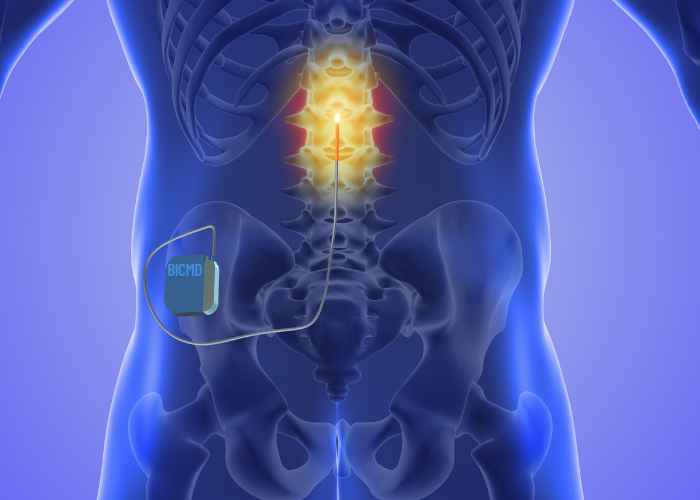
If a neck, back or spine condition or injury is keeping you from enjoying the freedom of a pain-free life, our physicians are committed to helping you feel better.
Click on “Get Started” to reach one of our orthopedic telemedicine experts.
Best in Class Shoulder Specialists
BICMD Reviews
“With the treatment options I received before my BICMD consultation, I had no interest in surgery. Speaking with my BICMD Expert gave me confidence, and I believe in his treatment suggestion.”