Expert knee care at your fingertips
You’re tired of living with chronic knee pain, but you want to avoid any unnecessary procedures. With access to the country’s best experts, you can get back to doing the activities you love.
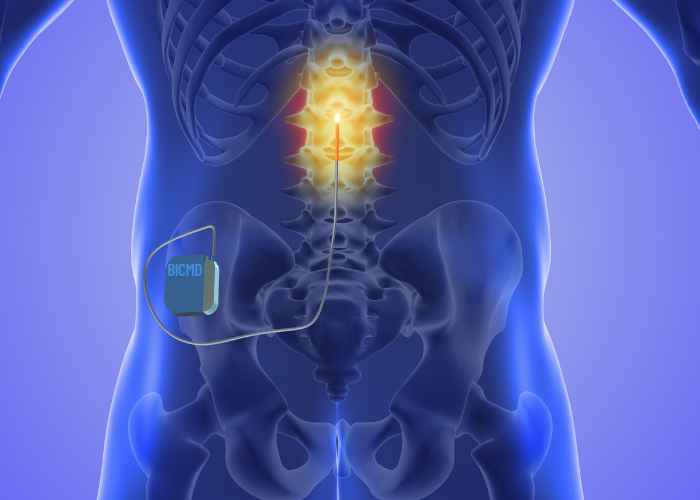
Feel completely confident in your journey toward knee health
Whether you need a second opinion or you’re just starting out, it’s time to work with a knee specialist at Best In Class MD. Find your condition or recommended treatment below and see how we can help.
This list contains some of our most commonly seen conditions and treatments, but it is by no means exhaustive. Our knee doctors handle the same wide variety of conditions and treatments that an in-person physician would.
If a knee condition or injury is keeping you from enjoying the freedom of a pain-free life, our physicians are committed to helping you feel better.
Click on “Get Started” to reach one of our orthopedic telemedicine experts.
Best in Knee Specialists
“I’ve now made a decision about my next steps and the BICMD platform truly fulfilled its promise to provide expert second opinions.”